CVS stops zepbound coverage and cites the high cost of weight loss drugs
Fox News Medical contributor Dr. Marc Siegel discusses Eli Lilly’s response to the “Claman Countdown” prescription drug outbreak.
CVS Caremarkone of the three major US pharmacy benefits managers (PBMs) has halted coverage for Eli Lilly’s popular weight loss drug Zepbound and blamed the drug for driving overall planning costs.
Originally developed for the treatment of type 2 diabetes, the GLP-1 product is now FDA approved for obesity under brand names such as Wegovy and Zepbound, and “contributes significantly to the overall planning cost,” CVS spokesman Philip Brand told FOX Business. According to Blando, removing drug coverage saves 10%-15% of clients year-on-year for clients who choose to cover obesity medications.
Zepbound, the brand name for Eli Lilly’s tilzepatide, was approved by the FDA in 2023 for chronic weight management in overweight adults with obesity or weight-related medical problems. Tilzepatide was already approved for the treatment of type 2 diabetes and was sold under the brand name Mounjaro.
Trump says drug prices will be reduced by up to 90%: What should you know?

The “Drive-Thru Pharmacy” sign will appear on Friday, February 7, 2014 outside the CVS Caremark Corp. store in Dallas, Texas, USA. (Getty Images/Bentorres via Getty Images/Bloomberg)
Zepbound was widely considered a game-changer in the fight against obesity after participants in late studies lost up to a quarter of their weight. From Wegovy.
Blando said the “significant high prices” for GLP-1 products set by the pharmaceutical company was “the single biggest barrier to patient access.”
“Many payers, including Medicare and numerous state benefits plans, have refused to cover GLP-1 for weight loss due to the high prices that are sustained and priced set by brand pharma,” he said.
However, there are still exceptions if the drug is considered a “medical need.” According to Blando, the exemption will be reviewed “on a case-by-case basis.”
CVS Caremark is a subsidiary of CVS Health Corp., which owns CVS pharmacy. As a pharmacy benefits manager, CVS Caremark essentially acts as a negotiator between pharmacies, insurance companies, and pharmaceutical companies. Prescription drugs supply chain. PBMs negotiate with drug manufacturers and pharmacies to determine how much the drug costs, which drugs will be available, and which drugs are part of the network.

Pedestrians will pass the CVS Caremark Corp. Store in New York, USA on Tuesday, April 30, 2013. CVSCaremarkCorp. is scheduled to release revenue data on May 1st.
The drug giants are critical of PBM and say their role needs to change. Eli Lilly previously told Fox Business that the only way to lower prices for US consumers is whether “there are fewer intermediaries themselves.”
Dr. Christopher McGowan, a gastroenterologist and obesity medicine expert, told the Fox business that CVS Caremark’s decision to reduce drug coverage is “deeply destructive for patients who are already stable and thriving with the drug.”
Low run with Ozempic or another weight loss medication? New trackers are useful
“We now find that insurance policies are nullifying medical judgments, forcing patients to switch to alternatives that are still effective but have been shown to lose less weight than Zepbound,” McGowan said.
McGowan emphasized that GLP-1 drugs “although they resemble paper, they are not actually interchangeable.” He said switching drugs could “be tough and reverse progress during the mid-journey period.”
“For many, this is not just an alternative, it is a high stakes change that can affect long-term outcomes. Introducing new side effects,“McGowan said.
According to McGowan, this exceeds the CVS care mark. McGowan is concerned that the decision with Zepbound “emphasizes a troubling trend” in that “financial agreements between benefits managers and drug manufacturers are increasingly shaping clinical decisions.”
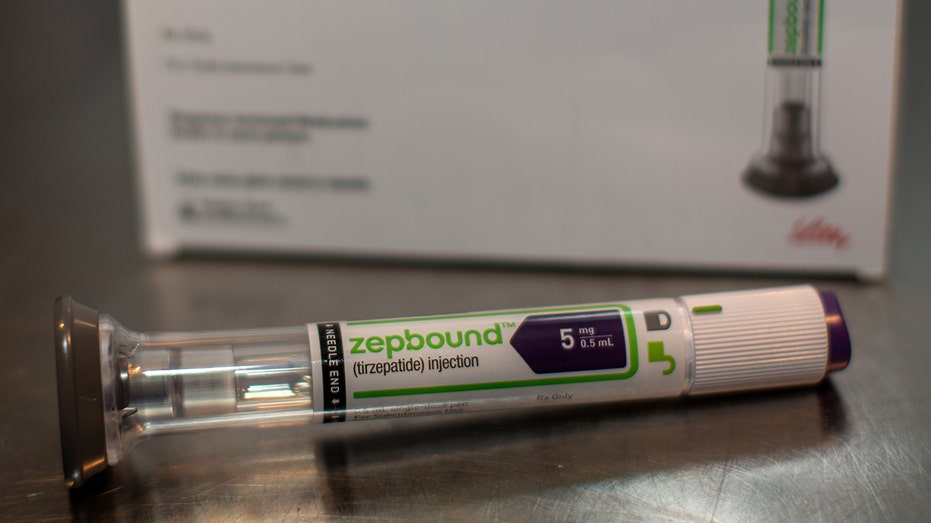
Eli Lilly & Co was placed in the Brooklyn Borough of New York, USA on Thursday, March 28th, 2024. Zepbound injection pen. (Getty Images/Shellby Knowles via Getty Images/Bloomberg)
This means that patients with fewer options aren’t the best for their health, he went on for a behind-the-scenes rebate transaction.
“Continuity is important in obesity care. Once a patient finds a working drug, it should be a priority to maintain its success,” he said. “Instead, progress is disrupted and patients are forced to navigate changes in treatment that they never wanted.”
Eli Lilly told Fox Business that the company is committed to ensuring patients have access to the care they need.
“Although not all CVS Caremark plans were affected, we have made a robust effort to actively communicate with many patients that may be affected through our support programme, and we have also added resources to our website.
Click here to get your Fox business on the go
If a customer loses coverage, Eli Lilly said he expanded access through LillyDirect’s self-paid pharmacy solution. This removes some third-party supply chain entities and third-party supply chain entities that provide patients without discounting compensation medications.
The pharmaceutical giant said patients who are prescribed Zepbound and who need access to it without having to enroll in health insurance will be able to get a single dose vial for around $500.





