I had one simple procedure to reduce the risk of fatal cancer for women. Here’s probably why you don’t know about it
I woke up from the surgical grogies with three slight incisions in my abdomen and a huge peace of mind. The fallopian tubes were slowly removed, because it was the best and perhaps only excluded, so Ovarian canceralthough rare, it is the most deadly gynecological cancer.
There is no way to detect ovarian cancer (the common misconception is that Pap smearbut that’s because cCervical cancer). This is mainly due to the relatively recent discoveries. Ovarian cancer forms about 80% of the fallopian tubes and is not easily reached or biopsy. Therefore, cancer is not discovered until it spreads beyond the tube. At that point, it is usually at a later stage, difficult to treat, with a treatment rate of 15%.
Cancer and pre-cancer lesions cannot be detected by blood tests either.
I myself didn’t know anything about this until 2023. I wrote it Ovarian Cancer Research Alliance (OCRA) created Sweep Recommendations: All women are genetically tested to know the risk of disease, and all women should consider having what is called opportunistic charectomy, regardless of their risk factors.
Since 2015, the strategy recruited by the American College of Obstetrics and Gynecology was thought to reduce the risk of ovarian cancer by up to 60%. After being based in the plain UK, it was adopted as a wide range of recommendations. Clinical trials Over 20 years, they tracked 200,000 women and found that screening and recognition of symptoms were not life-saving.
As Breast cancer survivorsthe idea of ovarian cancer could have been hanging out in my fallopian tubes. So when I had the opportunity to remove them during a recent minor abdominal surgery, I seized them.
Recovery from anesthesia – pain at the incision site and unpleasant bloating from the gas, and the surgeon pumped it into my belly, allowing her to see her path – let me relax for about a week while waiting for me for a month. But now I feel very relieved about my decision.
It especially started a public campaign on preventive dermatectomy in 2010, and is half-following around 80,000 people, who didn’t choose. resultIt was presented at the American Cancer Research Association conference in March 2024 and at the recent annual general meeting of the Gynecological Oncology Society.
“There’s very little in medicine that offers 80% risk reduction,” says a study from Gillian Hanley, an associate professor of obstetrics and gynecology at the University of British Columbia. “That’s amazing.”
So why don’t more women know about it?
Efforts to raise awareness of opportunistic major skin resections
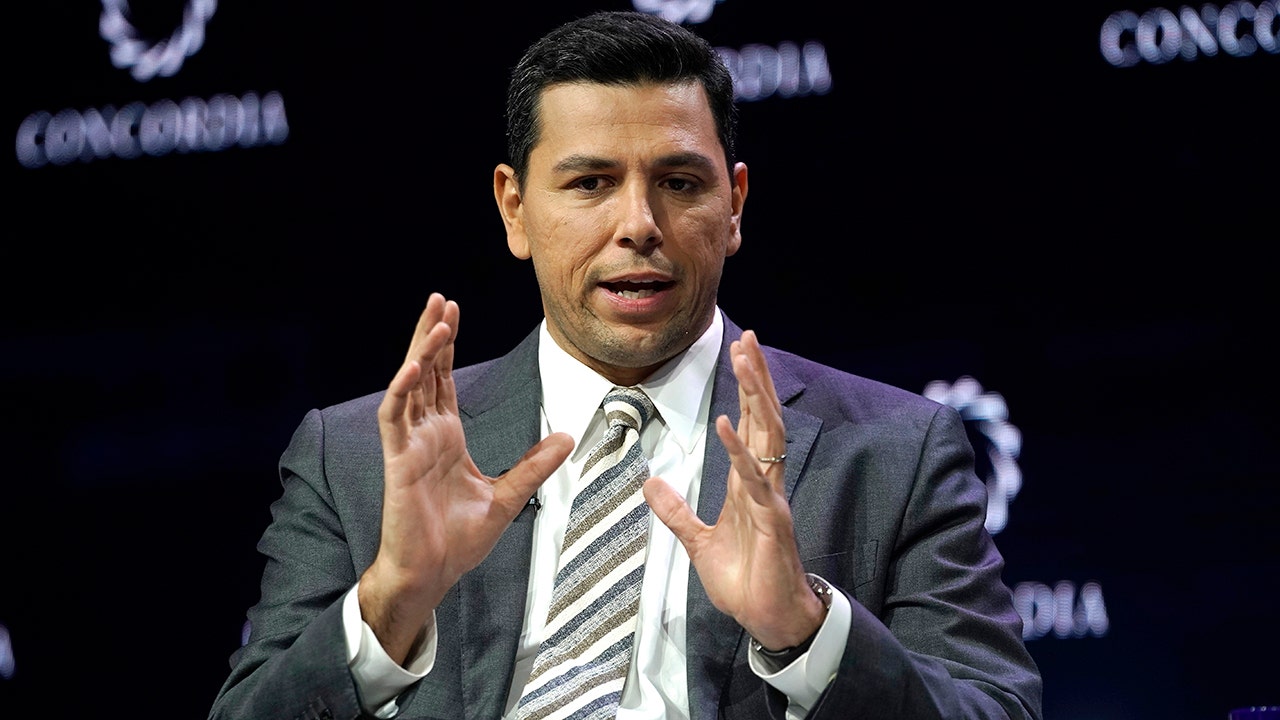
Dr. Rebecca Stone, gynecological oncologist at John Hopkins Medicine, is the leader in an effort to uncover the language of ovarian cancer prevention, diagnosed by about 20,000 Americans a year and killed more than 12,000 people. Seeing so many patients die is what awakened the surgeon at night.
She began making her mission an opportunistic, large-scale extraction procedure that began in 2023. At that time, the results of the UK trial prompted organizations like OCRA to make headlines with new recommendations.
“When it all came out, I was like, ‘Oh, amazing. Thank God.’ But I was like, ‘I’m not ready yet,'” Stone says. luck.
That’s because there was no infrastructure to make cock excision the norm. While women wait in the gynecologist’s office, there is no educational material for women to cause leaves, and there is no awareness among gynecologist surgeons about providing procedures, and not even aware of claim codes covered by insurance for the procedure.
At about the same time, Stone was asked to attend a meeting of the Scientific Advisory Committee. Break through cancera joint effort between top researchers and doctors to prevent and treat the most deadly cancers. Someone asked her if she knew how to cure ovarian cancer.
“I was trying to believe in me. We sometimes get lucky, but most of the time I bury the patient,” she says. “Then I said, ‘But we know how to prevent that.'” At that time, she recalls, ‘people’s hair was blown away.’ Even the top cancer mind of the call had never heard of the effectiveness of zalping resection.
That call led to the creation of a new break initiative for cancer, Interception of ovarian cancer, It aims to improve detection of pre-fallopia cancers and to expand charectomy as a preventive tool within the general population. Stone has already managed to work with the Centers for Disease Control and Prevention to create specific billing codes for the procedure, and is currently preparing to launch the Outmart Ovarian Cancer Campaign with Dr. Kara Long, a commemorative Sloan Kettering gynecological surgeon.

“Remember when smoking cessation was a cancer prevention strategy that left people behind? I think signs and ads are what you need here,” says cancer biologist Tyler Jacks, who breaks through the president of cancer.
“This is a systematic issue that brings true cultural change to solve within and beyond the medical community,” adds Audra Mora, president and CEO of OCRA, about the slow adoption of carbonised excision. “We know it’s not as widely adopted as possible.”
Certainly there are still barriers to this effort. This includes ways to present the issue to sensitivity in some communities of colours that bring about historic US burdens. Forced sterilization; until Vancouver’s findings are based on historical data, it convinces some surgeons that there is ample evidence behind it. The idea of surgical prevention itself can also be uncomfortable.
However, Stone quickly points out, as another surgical prevention is accepted as the standard. “It’s called colonoscopy,” she says. “And the risk of colonoscopy is much higher,” including the possibility of intestinal perforation. “And what do you guess? You have to start over again in five or ten years.” She argues that Salpingectomy is one thing, and “much more cost savings” in the long run.
Furthermore, Hanley said, “Of course, it’s not suggesting that everyone with fallopian tubes needs to be surgically removed. That’s by no means a recommendation. It’s a surgical intervention, and surgery isn’t risk-free.” However, she considers it “exciting.” “For many years, we haven’t had much cancer prevention that focuses on lifestyles. It focuses on diet, exercise, environmental exposure to carcinogens, and the real challenges of change.”
Is Salpingectomy perfect for you?
Those who have completed their child or who have not planned on having another abdominal surgery are candidates for opportunistic large dermatectomy, such as approved resection, gallbladder removal, or hysterectomy.
“What we’re really saying is if you’re already undergoing some kind of surgery, you’re already having some benign disease you’re treating, and the surgeon is already there. Adding this to another procedure means there’s compelling evidence that you won’t change your risk at all compared to what you already risk the surgery,” says Hanley.
If you haven’t had another surgery and want to remove the fallopian tube anyway, you can technically choose it as the route to sterilization (instead of tubal ligation).
In a woman High risk-Stone says, “We should recommend standalone group resection to reduce the risk,” including increasing the risk of ovarian cancer from 1% to 5%, compared to 1% who have genetic mutations such as BRCA1 and BRCA 2. They may also consider oophorectomy (removal of the ovaries), she adds.
The long-term risk of salpingectomy is not known, if any, but she says that ovarian tubes do not serve known purposes beyond breeding, and thus are likely to produce important hormones beyond menopause, as ovarian tubes do not serve known purposes, as opposed to the ovaries.
I chose to maintain the ovaries. But these decisions are of course very personal. I didn’t think I would be someone who would undergo elective surgery in the first place, but the statistics convinced me.
As for Stone, she says she spent time in the operating room trying to save a patient “with this horrible illness” to give up consciousness.
“I’m going to spend the rest of my life trying to get this information out there,” she says.
Details about women and cancer:
- Three women in three skip daily appointments and put themselves at high risk of cancer
- There is no such thing as early detection in ovarian cancer. Here’s what you need to learn from tennis: Chris Evert’s fight against illness
- Women will be notified of breast density after mammograms. This is what should happen next
This story was originally introduced Fortune.com